A Guide to the Management of Paediatric Dental Trauma
Dr. Kunal Patel, Specialist in Paediatric Dentistry
In this article, our Specialist Paediatric Dentist in Fulham Dr. Kunal Patel shares a formal guide to ‘The Management of Paediatric Dental Trauma.
Aim:
To improve your knowledge and confidence in managing paediatric traumatic dental injuries (TDIs)
Objectives:
Be able to
- Obtain a history and examine a patient with dental trauma
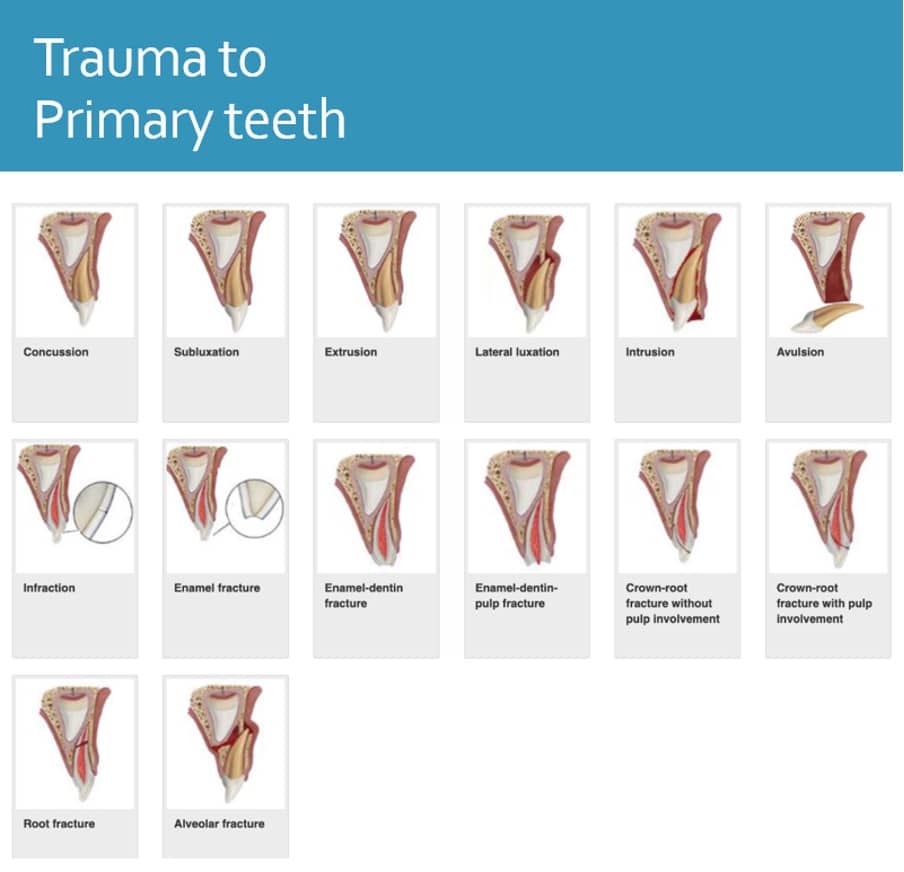
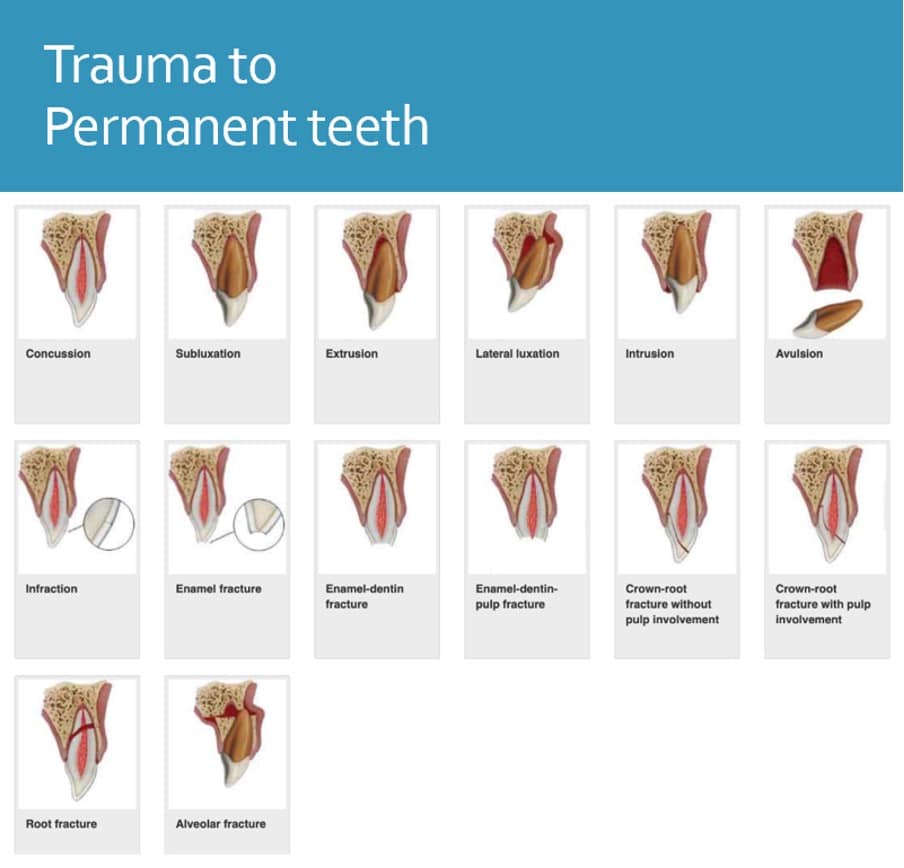
- Establish and document diagnosis of dental injuries
- Understand the management of dental trauma
- Follow the latest guidance
- Improve outcomes for paediatric patients
Introduction
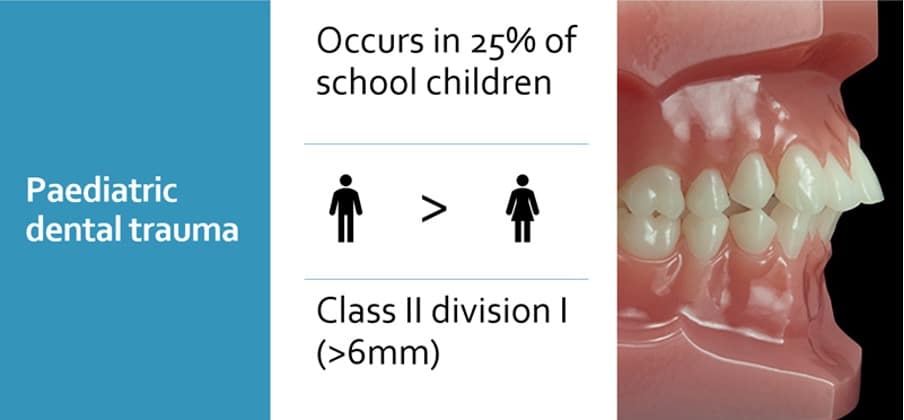
Trauma to permanent teeth most commonly occurs in children & young adults
Crown fractures & luxations are the most common
Appropriate diagnosis, treatment and follow-up are imperative to achieve favourable outcomes
Loss of permanent anterior teeth can have a lifetime of consequences
Challenges with Paediatric patients
- Heightened emotions
- Difficulty examining young children
- Existing dental anxiety or phobia
- Moisture control when splinting
- Time constraints
- Operator Confidence/Experience
Consent
Ensure: Ensure you obtain informed consent from an adult with parental responsibility
Provide: Provide emergency treatment in the patient’s best interest
Seek: Seek second opinion if unsure
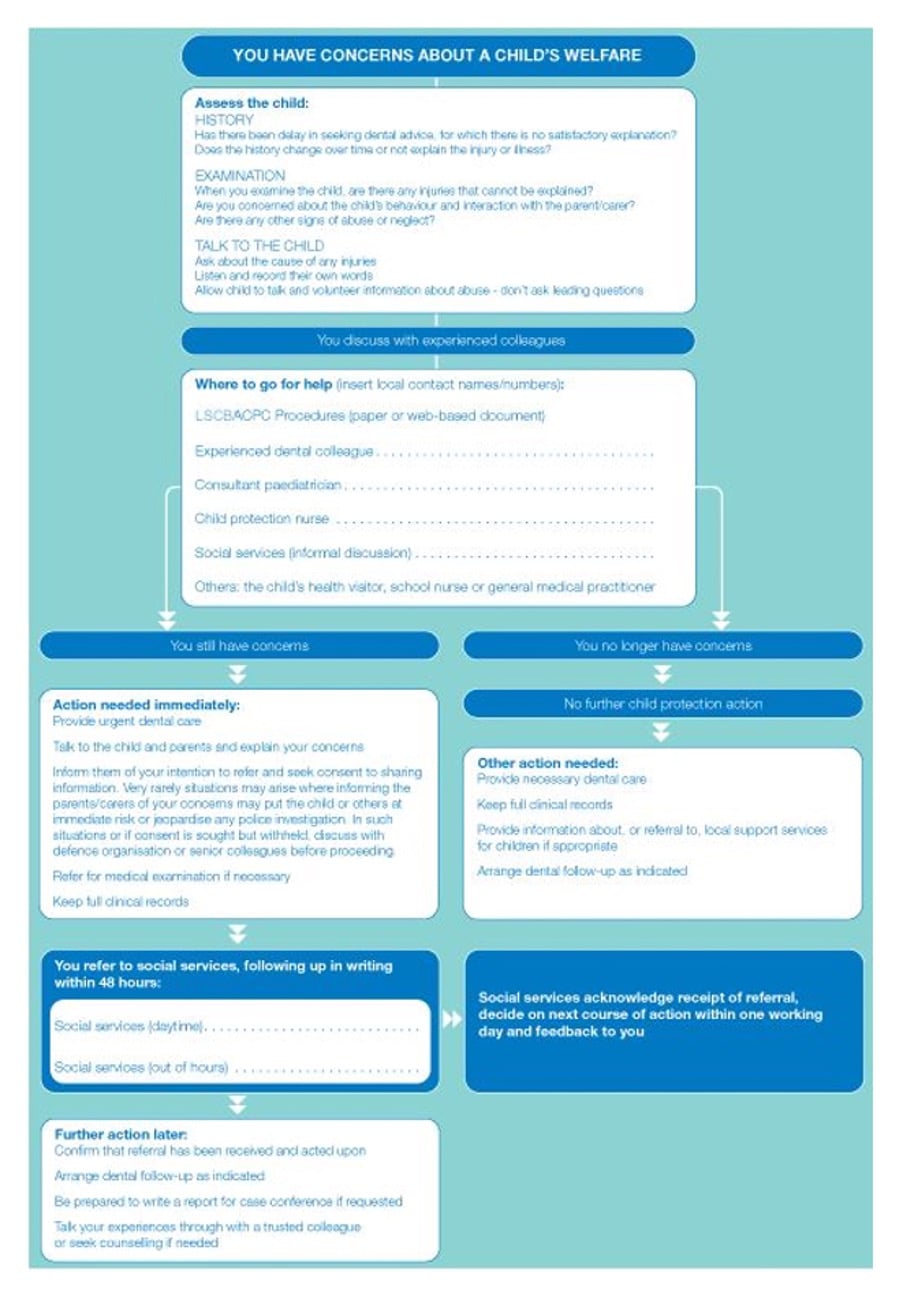
Safeguarding
- Follow your practice safeguarding children policy
- Any non-accidental injury concerns contact social services
- MASH duty officer will be able to listen and act on any concerns you may have
- You may be picking up a small detail of a wider picture of child neglect
- Documenting a thorough history is essential!
History taking
- Patient attended with?
- Parental responsibility & consent
Trauma history
- Loss of consciousness / nausea / vomiting / amnesia / dizziness
- Other injuries
- Change to the bite?
- When did the injury occur? (date & time)
- How did the injury occur?
- Where did it take place?
- Was the event witnessed?
- Location of any missing fragments/teeth
- Previous traumatic injury?
- Police involvement
Medical history
- Immunocompromised?
- Bleeding disorders?
- Allergies?
- Vaccination status – Tetanus
Social history
- Who lives with the child?
- Which school do they go to?
- Do they have a social worker?
- Document any concerns you may have
Dental history
- Previous experience of LA/Sedation/GA
Examination
Extra oral
Swellings, lacerations (debris), bruising
Eye movements and pupillary reflexes, limited mouth opening, palpate facial bones
Intra oral
Bruising, lacerations, swellings, step deformity in occlusal plane, dental injuries, measure displacement of teeth (mm)
Tooth colour, mobility, percussion, sensibility (Endofrost/EPT)
Radiographic assessment
Occlusal & Periapical
Photographs
Ask parent if photo of patient smiling beforehand
E.g. Palatal luxation could be natural position
In which 4 scenarios would you not re-implant teeth?
1 – Primary tooth
2 – Other injuries are severe and warrant preferential emergency treatment
3 – Medical history (i.e. immunosuppression in acute lymphoblastic leukaemia)
4 – Immature permanent tooth with short apex and prolonged dry time (psychological impact
https://dentaltraumaguide.org/free-dental-guides/primary-teeth/
Considerations for primary tooth trauma
- Eating/drinking
- Pain
- Signs of infection
- Inhalation/airway risk
- Co-operation
- Reassurance
Primary teeth – Management
Keep things simple:
- Concussion and subluxation : Reassurance, soft diet
- Luxation injuries : Extraction if in traumatic occlusion
- Avulsion : DO NOT REIMPLANT
- Uncomplicated Crown Fracture : GIC dressing if co-operative and monitor
- Complicated crown fracture : Extraction
- Root fracture : If apical 1/3 leave and monitor, otherwise extract
Case 1
- 18 month old child
- MH: Fit and well
- Attended with mother
- Fell off chair and hit a table
Describe what can you see?
Things to remember – Case 1
- How did it happen? Ensure to take a thorough history to rule out NAI
- Risk of damage to permanent tooth germ
- If treatment is required – are they likely to allow for treatment under LA or inhalation sedation
- Parents / carers may also be traumatised by the event
What clinical signs would you look for?
Clinical signs – Case 1
Extra-oral injuries including lip and skin lacerations
Lacerations/ haematomas of the: lips, oral mucosa, gingivae, frenulum
Bleeding from the sulcus surrounding the injured tooth indicate damage to the PDL
Contusions of lower lip or chin are seen more frequently with intrusion injuries
Intruded incisor may not be visible if fully intruded
May be concomitant luxation injuries
Management – Case 1
Immediate treatment:
Re-assure parent and child
Tailored oral hygiene instruction – soft toothbrush, chlorhexidine gel
Analgesia advice
Warn of change in shape of crown or root; colour; eruption timings
Referral to paediatric specialist if concerns
Long term treatment:
The tooth should be allowed to spontaneously reposition itself, irrespective of the direction of displacement
1 week – Clinical examination.
6-8 weeks – Clinical examination.
6 months – Clinical and radiographic examination.
1 year – Clinical and radiographic examination, clinical and radiographic monitoring until eruption of the permanent successor
Spontaneous improvement in the position of the intruded tooth usually occurs within 6 months, in some cases, it can take up to 1 year
Dental Trauma Guide – $33 per year = £24 https://dentaltraumaguide.org/free-dental-guides/
Updated IADT Guidelines (2020) https://doi.org/10.1111/edt.12574
Permanent teeth – Management summary
Concussion:
Soft diet and advice
Subluxation:
Soft diet and advice +/- 2 week splint
Crown fracture:
Uncomplicated – composite bandage
Complicated – Cvek/Extirpate
Crown root fracture:
Apical or Mid 1/3 – splint 4 weeks and monitor pulp vitality
Coronal 1/3 – splint for up to 4 months
Lateral luxation:
Reposition tooth under LA – disengage from locked position
Splint for 4 weeks
Review
Extrusive luxation:
Reposition tooth under LA
Splint for 2 weeks
Review
Intrusive luxation:
Immature apex
Allow spontaneous re-eruption (regardless of degree of intrusion)
If no eruption in 4 weeks – orthodontic extrusion
Mature apex
Mild <3mm : Spontaneous re-eruption (8wks), consider orthodontic/surgical repositioning
Moderate 3-6mm : Repositioning surgically / orthodontic extrusion
Severe >6mm : Repositioning surgically / orthodontic extrusion
RCT at 2 weeks
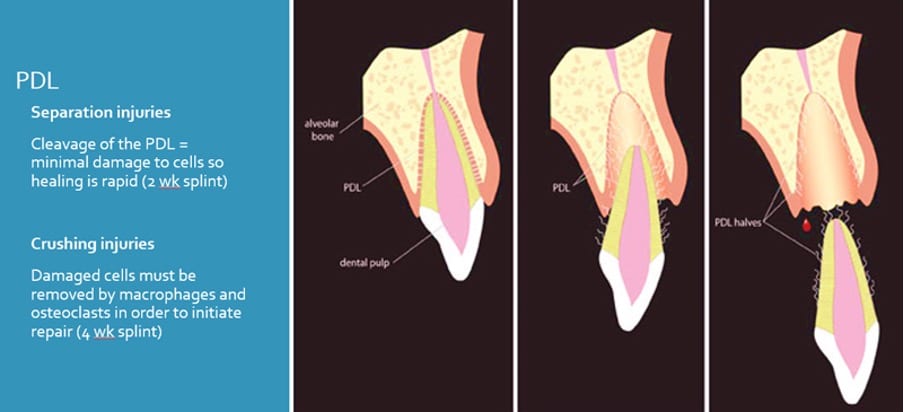
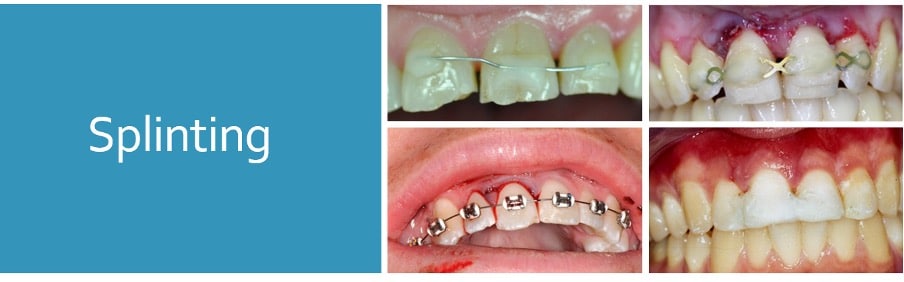
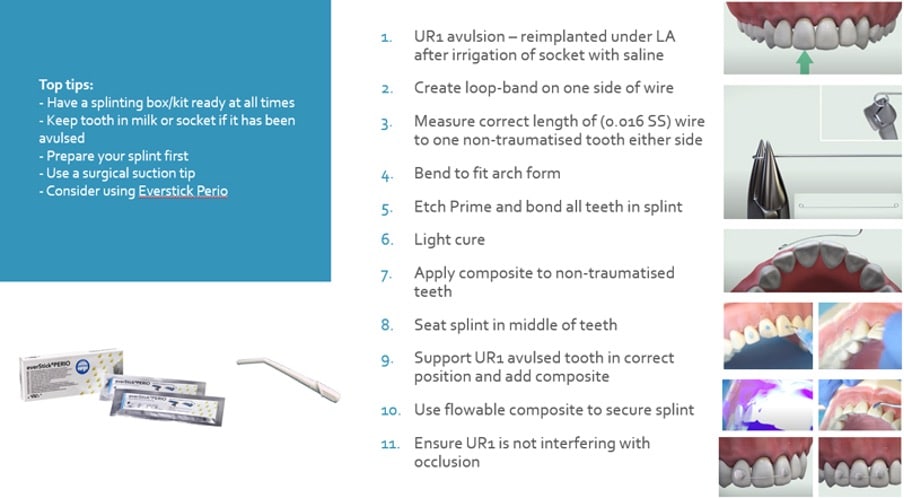
Splinting
Ideal requirements
- Secure
- Easily applied and removed
- Stabilise tooth in correct position
- Allow physiologic tooth mobility
- Allow pulp sensibility testing and endodontic access
- Allow adequate OH
- Avoid interference with occlusal movements
- Provide comfort
Types
- Composite and wire*
- Orthodontic wire and bracket*
- Fibre splints (Everstick)*
- Titanium trauma splints
- Composite splints
- Suck-down splints
- Buccal (usually)
- Flexible (0.016” SS wire)
- Passive
- One non-traumatized tooth either side of affected tooth/teeth
- Keep away from gingival margin
Aftercare instructions
- Avoid participation in contact sports
- Maintain a soft diet for up to 2 weeks, according to the tolerance of the patient
- Brush their teeth with a soft toothbrush after each meal
- Use a chlorhexidine (0.12%) mouth rinse twice a day for 2 weeks
Case 2
8-year-old attends following an avulsion UL1 at school. He attends with his school teacher who has brought the tooth in milk. She reports that the tooth has been in milk for 45 minutes. The tooth has an open apex.
What are you concerns?
Concerns – Case 2
Consent
Safeguarding / NAI
Act in patient best interest
Condition of tooth
Medical background
Total extra-oral time (inc. dry time)
What is your immediate management?
Contact parents
Medical history and history of trauma
Clean the root surface with saline
LA
Examine the alveolar socket. If there is a fracture of the socket wall, reposition it with a suitable instrument
Irrigate the socket with sterile saline to remove coagulum and debris
Replant the tooth slowly with slight digital pressure
Verify normal position of the replanted tooth clinically and radiographically
Apply a flexible splint for up to 2 weeks
Suture gingival lacerations, especially in the cervical area
Administer systemic antibiotics
Amoxicillin/penicillin (first line)
Tetracycline – Doxycycline BD 7 days (<12 year – Consider risk of discolouration)
Tetanus
What is your long-term management?
Patient instructions:
Avoid participation in contact sports
Soft food for up to 2 weeks
Brush teeth with a soft toothbrush after each meal
Use a chlorhexidine (0.12%) mouth rinse twice a day for 2 weeks
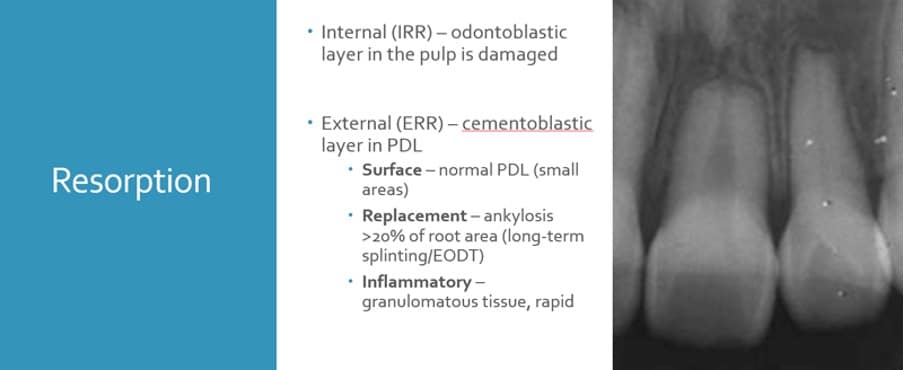
Warn patient of future: monitoring with GDP or specialist, root canal treatment, resorption, ankylosis, need for replacement
Long term Follow-up:
Refer to Paediatric Specialist
Root canal treatment should be avoided unless there is clinical or radiographic evidence of pulp necrosis
Splint removal and clinical and radiographs after 2 weeks
Clinical and radiographic review after
4 weeks, 3 months, 6 months, 1 year and then yearly thereafter
Case 3
12 year old attends with his grandmother following a fall at school 4 days ago. He reports that he is in a lot of pain and is very nervous. Clinical and radiographic examination shows a clear palatal luxation UL1
What are your concerns?
Consent
Attempt to contact parent and document
Act in patients best interest
Patient Gillick competent?
Who has PR? Any social worker involvement?
Delayed presentation?
Who was present at time of injury
Does grandmother look after him often
What is your management?
Full history, clinical and radiographic examination, sensibility testing
Reposition UL1 and splint
Ensure tooth is not interfering with occlusion
Treatment options
LA/RA
Follow up
Ensure patient has follow-up in place
Clinical and radiographic evaluations are necessary: after 2 wk
after 4 wk S+, 8 wk, 12 wk, 6 mo, 1 y, then yearly for at least 5 y
Patients to return if any unfavourable outcomes
Risks:
Resorption
Ankylosis
Loss of tooth
Discolouration of tooth
RCT/Extraction
Interdisciplinary management
Factors which affect outcomes
Maturity of root
Viability of PDL
EODT (avulsion permanent teeth)
Degree of trauma
Factors which determine favourable outcomes
Appropriate Diagnosis
Treatment Planning
Timing
Follow-up
Discussion…
- 8 year old male
- Fell off his scooter and hit the concrete floor
- Referred from a district general hospital
- Cleared of head injury
- Immediate management completed
What has been done well?
What could be improved?
Dental management
History, examination & radiographs
Ask parents for photographs before accident
Keep avulsed tooth in milk/sterile saline
Administer LA
Reposition alveolar socket
Reimplant tooth and reposition displaced teeth and splint
Refer for follow-up care
Key messages
- Treat as soon as possible for better outcomes
- Consent – Check who patient has come in with
- Safeguarding – check social worker and NAI
- If in doubt – Refer
- Ensure follow up is in place!
References
https://www.dentaltrauma.co.uk/File.ashx?id=15336
https://bda.org/childprotection/Recognising/Pages/Physical.aspx
https://dentaltraumaguide.org/free-dental-guides/permanent-teeth/
Fouad, AF, Abbott, PV, Tsilingaridis, G, et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 2. Avulsion of permanent teeth. Dent Traumatol. 2020; 36: 331– 342. https://doi.org/10.1111/edt.12573